Understanding Depression, Personality Plasticity, and the Role of Structured Internal Value Hierarchies (SIVHs) in Employee Well-Being
First published: 04.03.2025
Leading author: William Parvet
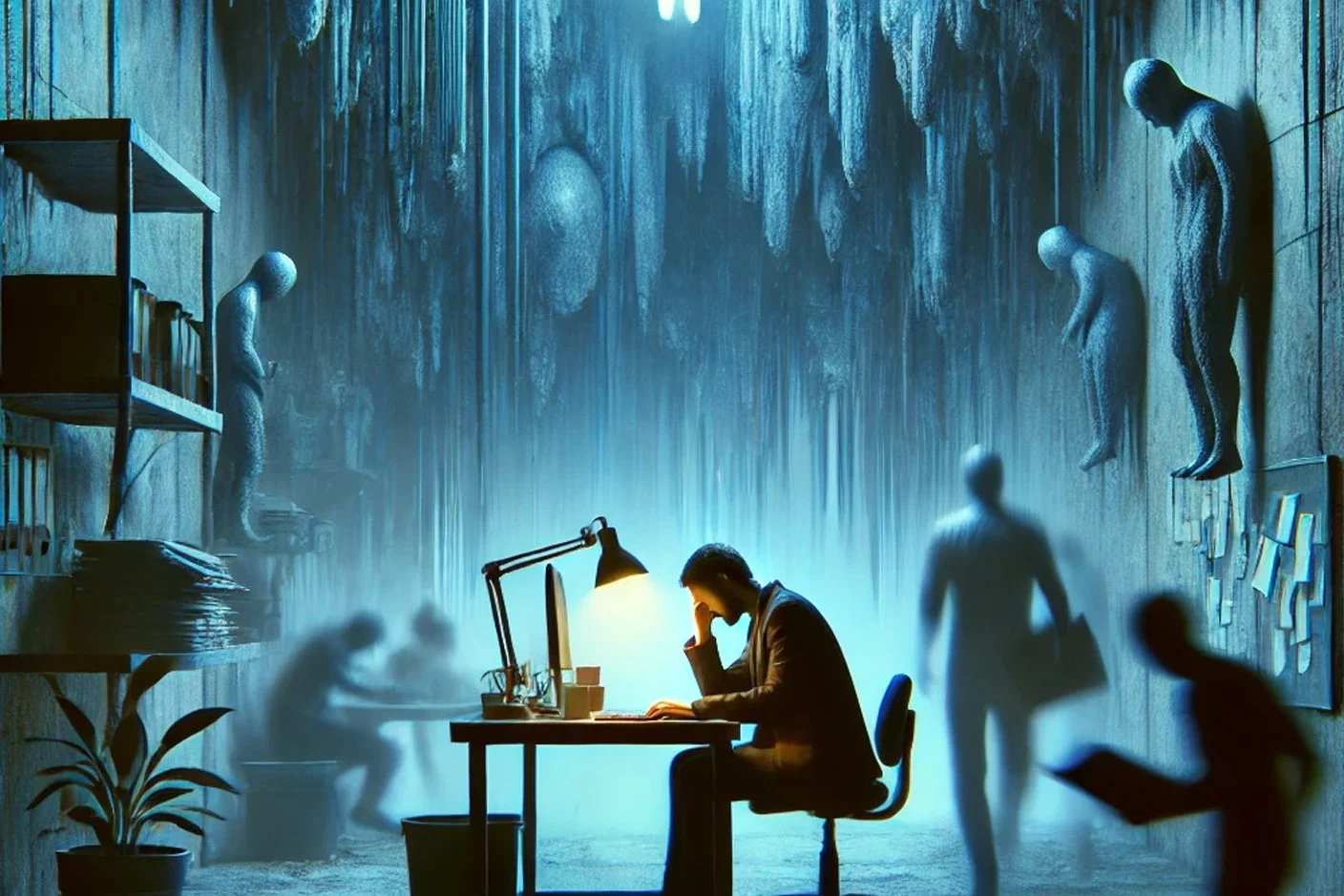
Depression is more than a temporary emotional state — it fundamentally reshapes cognitive function, motivation, and an individual’s interaction with their environment. In the workplace, its effects extend beyond personal struggles, influencing productivity, decision-making, and team dynamics. While traditional approaches to managing workplace mental health focus on external interventions such as leadership style, workload adjustments, and support systems, SelfFusion takes a deeper, more structured approach: understanding the internal neurochemical and cognitive mechanisms that define an individual’s resilience and adaptability.
This article explores the nature of depression and its effects on employees, but more importantly, it examines how Structured Internal Value Hierarchies (SIVHs) — a core principle in the SelfFusion framework—can influence key personality traits, particularly openness to ideas and assertiveness. SIVHs provide a systematic way to align intrinsic motivation with external challenges, making it possible to reshape behavioral responses and cognitive flexibility in the workplace.
At the core of this process is neurochemistry, which plays a pivotal role in personality expression and adaptability. Certain traits exhibit high plasticity, meaning they can be systematically influenced when individuals engage in structured cognitive and behavioral interventions. By leveraging SelfFusion models, we explore how SIVHs can be applied to optimize decision-making, assertiveness, and creative problem-solving — turning what is traditionally seen as personality limitations into opportunities for controlled transformation.
In essence, this article challenges the notion that personality is a fixed determinant of workplace performance. Instead, we introduce a science-backed approach that leverages neurochemical flexibility and structured value alignment to enhance employee well-being, adaptability, and performance.
Depression is a multifaceted condition with a strong neurochemical foundation. While serotonin is commonly associated with depression, a broader understanding reveals a complex interplay between neurotransmitters, hormones, immune system activity, and structural brain changes.
Chemical breakdown of Depression
Serotonin
One of the primary neurotransmitter imbalances observed in depression involves serotonin, which plays a crucial role in mood regulation, emotional stability, and sleep. Low levels of serotonin are often linked to depressive symptoms, and a deficiency in tryptophan, its precursor, can exacerbate mood disorders. The effectiveness of selective serotonin reuptake inhibitors (SSRIs) in treating depression highlights serotonin’s significance.
Dopamine
However, dopamine dysfunction also plays a critical role, particularly in anhedonia—the inability to experience pleasure. A reduction in dopamine activity in the mesolimbic pathway leads to diminished motivation and reward sensitivity. In some cases, particularly in atypical depression, dopamine function may be preserved or hypersensitive, contributing to mood reactivity. Similarly, norepinephrine levels are often low in depressive individuals, which results in fatigue, low energy, and cognitive impairment due to reduced activity in the locus coeruleus. Serotonin-norepinephrine reuptake inhibitors (SNRIs) target this neurotransmitter to enhance alertness and focus.
GABA
Beyond the monoamine system, glutamate and GABA also influence depressive symptoms. Low glutamate levels contribute to impaired synaptic plasticity and cognitive dysfunction, while treatments like ketamine, an NMDA receptor antagonist, have shown rapid antidepressant effects by enhancing glutamate transmission. At the same time, GABA, the brain’s primary inhibitory neurotransmitter, is often reduced in depression, leading to heightened stress sensitivity and a decreased ability to cope with adversity. Acetylcholine also plays a role, as its overactivity is linked to excessive rumination and persistent negative thoughts. An imbalance in muscarinic receptor activity may contribute to this persistent cognitive rigidity.
Cortisol
Depression is closely tied to hormonal dysregulation, particularly within the hypothalamic-pituitary-adrenal (HPA) axis. Chronically elevated cortisol is one of the most consistent findings in depressed individuals. Excessive cortisol secretion negatively affects brain structures such as the hippocampus, leading to impaired memory and emotional regulation. It also increases amygdala activity, resulting in heightened fear responses, while suppressing prefrontal cortex function, which weakens decision-making and impulse control. This overactive stress response disrupts serotonin and dopamine synthesis, worsening mood symptoms.
Thyroid Dysfunction
Additionally, thyroid dysfunction, particularly hypothyroidism, has been associated with depressive states, as lower levels of T3 and T4 contribute to sluggishness, cognitive fog, and decreased energy. Some individuals exhibit thyroid hormone resistance, which complicates their ability to regulate mood. Another hormone, oxytocin, which is involved in social bonding and emotional warmth, is often reduced in depressed individuals, leading to social withdrawal and feelings of isolation.
Inflammation
Inflammation is increasingly recognized as a key player in depression. Elevated levels of pro-inflammatory cytokines such as TNF-α, IL-6, and IL-1β can induce sickness behavior, characterized by fatigue, low motivation, and anhedonia. Chronic inflammation also activates microglia, the brain’s immune cells, which can lead to excessive synaptic pruning and neurodegeneration. Additionally, inflammation influences serotonin metabolism by shifting tryptophan toward the kynurenine pathway, reducing its availability for serotonin synthesis and increasing the production of neurotoxic metabolites that further impair brain function.
Prolonged Depression
Structural and functional changes in the brain further contribute to depressive symptoms. The hippocampus, a key region involved in memory and emotional regulation, tends to shrink in individuals with prolonged depression, exacerbating cognitive difficulties. At the same time, the prefrontal cortex exhibits reduced activity, weakening emotional control and executive function, while the amygdala becomes hyperactive, amplifying fear and negative emotional processing. Dysfunction within the striatum, particularly in the dopamine system, further reduces pleasure and motivation, reinforcing a cycle of disengagement and despair.
Gut-Brain connection
The gut-brain axis and metabolic factors also play an important role in depression. Dysbiosis, or an imbalance in gut microbiota, affects serotonin and dopamine synthesis, as gut bacteria are involved in neurotransmitter production. A compromised gut barrier, often referred to as leaky gut syndrome, increases systemic inflammation, which, in turn, exacerbates depressive symptoms. Metabolic dysfunction, including insulin resistance and metabolic syndrome, can further contribute to cognitive sluggishness and mood instability, highlighting the interconnected nature of depression and overall physiological health.
Depression is not merely a disorder of low serotonin but rather a condition influenced by multiple biological systems. The combination of neurotransmitter dysfunction, chronic stress and hormonal imbalances, immune system activation, and structural brain changes creates a self-reinforcing cycle that makes recovery challenging. While traditional treatments like SSRIs address one component, newer approaches — including ketamine therapy, anti-inflammatory interventions, and metabolic treatments — offer more comprehensive solutions by targeting the broader neurochemical landscape of depression.
Using SIVHs to Counterbalance Depression
When utilizing Structured Internal Value Hierarchies (SIVHs) as a tool to mitigate depression, it is crucial to move beyond the intuitive focus on neuroticism alone. While it is evident that modifying volatility (emotional reactivity) and withdrawal has a notable impact on individuals prone to neuroticism, interventions such as SIVH developmenttend to have a modest but meaningful influence on depressive symptoms. We will examine these effects in detail below.
Volatility (Emotional Reactivity) and Depression
Depression and depressive states have a direct connection to SelfFusion’s model and the role of SIVHs in regulating emotional reactivity. The core personality factor in depression is neuroticism, which is strongly linked to serotonin levels. As discussed in various SelfFusion articles, neuroticism contributes to emotional instability, excessive worry, and heightened negative affect, all of which amplify depressive tendencies.
Emerging research suggests that increased orderliness, which can be cultivated through SIVH implementation, has the potential to influence serotonin regulation and reduce depressive episodes (DeYoung et al., 2010). By incorporating structured value-based routines, individuals may experience greater emotional stability and a reduction in the intensity and duration of depressive states.
Furthermore, studies have shown that structured worldviews, such as those created by SIVHs, help individuals develop a greater sense of control and meaning, which are protective factors against depression (Kashdan & McKnight, 2013).
Anxiety and Avoidance
High withdrawal behaviors — manifested as social avoidance, excessive rumination, and chronic worry—are strongly linked to persistent depression. Avoidance prevents engagement with rewarding experiences, leading to increased anhedonia (the inability to feel pleasure) and reinforcing depressive symptoms.
Through repeated observations, we have seen that the implementation of a clear SIVH can retrain the avoidance response by shifting focus toward higher-order goals and structured engagement with the world. Research in cognitive behavioral therapy (CBT) suggests that controlled exposure to positive experiences over time can lower withdrawal tendencies, significantly reducing depressive symptoms (Hofmann et al., 2012).
Similarly, self-determination theory supports the idea that intrinsic motivation and structured value systems can help override avoidance behaviors and promote greater engagement in meaningful activities (Deci & Ryan, 2000).
Conscientiousness: High Impact, Limited Plasticity
Although higher conscientiousness is often considered a powerful counterbalance to neuroticism, the opportunities for modifying orderliness and industriousness remain limited due to their relatively low plasticity.
While individuals may intellectually recognize the benefits of increasing conscientious traits, the practical implementation of such changes is challenging. Industriousness and orderliness—the two primary facets of conscientiousness—tend to be highly stable personality characteristics, shaped by genetics and long-term habitual patterns (Roberts et al., 2006).
However, if motivation aligns with existing personality traits and sub-traits, an SIVH can exert some influence by reinforcing goal-oriented behavior and structured decision-making. Research on personality plasticity suggests that behavioral interventions and structured belief systems can produce small but meaningful shifts in conscientiousness, particularly when supported by self-determined motivation (Hudson & Fraley, 2015).
Thus, while the impact of an SIVH on conscientiousness is significant, its modifiability remains constrained by biological and cognitive limitations.
Politeness and Depression: The Role of SIVHs
The effect of politeness on depression can be considered moderate to high, as excessive politeness is associated with low assertiveness, difficulty setting boundaries, and social submissiveness. These tendencies can increase stress-induced depression, particularly in individuals who struggle with self-advocacy.
Politeness, Assertiveness, and Depression
Studies have shown that high agreeableness, particularly in the form of excessive politeness, can lead to increased social stress and greater susceptibility to burnout due to an overemphasis on pleasing others at the cost of personal needs (Rosen et al., 2016). This aligns with findings that low assertiveness contributes to higher levels of depression and anxiety, as individuals with weaker boundary-setting abilities are more prone to emotional exhaustion (Kashdan et al., 2009).
Strengthening boundary-setting skills and fostering constructive assertiveness can reduce the depressive impact of excessive agreeableness. While SIVHs can aid in developing stronger internal principles, politeness—like most personality traits—tends to be relatively stable over time (Roberts et al., 2007).
Compassion and Its Limited Plasticity
Within agreeableness, compassion is even less malleable than politeness. Studies suggest that compassion is deeply tied to biological predispositions and early socialization, making it one of the least plastic personality subtraits(Kandler et al., 2014).
However, empirical observations suggest that one can replace the emotional experience of compassion with a rational understanding of its necessity. For example, in family contexts, individuals who may not naturally feel strong compassion can intellectually grasp its importance and act accordingly. This cognitive reframing allows for functional improvements in social behavior, even when emotional plasticity is low (Decety & Cowell, 2014).
Openness to Experience: Sufficient Plasticity but Mixed Effects
Openness to Experience is a double-edged sword when it comes to mental health and depression. While high openness is associated with creativity, intellectual curiosity, and adaptability, excessive openness can lead to existential anxiety, excessive rumination, and emotional instability, increasing vulnerability to depression.
The Dual Nature of Openness
Positive Effects: High openness fosters flexible problem-solving, adaptability, and creative engagement, all of which can contribute to psychological resilience. Individuals who are intellectually curious and open to new perspectives are often better equipped to reinterpret negative experiences in a constructive manner (Kaufman et al., 2016).
Negative Effects: Excessive openness can lead to overthinking, existential uncertainty, and persistent rumination, all of which have been linked to depression and anxiety disorders. High openness without emotional regulation may result in increased psychological distress due to a heightened sensitivity to uncertainty and abstract concerns (DeYoung et al., 2010).
Plasticity and the Role of SIVHs
Among the Big Five traits, openness has moderate plasticity, meaning it can be shaped through intentional interventions (Roberts et al., 2017). A key strategy to counteract the depressive impact of excessive openness is practicing focused thinking rather than free-associative rumination.
Structured thinking, guided by an SIVH, helps channel intellectual curiosity toward goal-oriented reasoningrather than aimless speculation.
Philosophical and existential concerns—which often contribute to anxiety in highly open individuals—can be anchored within a structured value hierarchy, reducing uncertainty and promoting stability.
Cognitive techniques such as metacognitive training (learning to monitor and control thought patterns) have been shown to reduce maladaptive rumination, which is often exacerbated by high openness (Wells, 2009).
Sufficient Plasticity and Significant Effect: Extraversion and Depression
Extraversion plays a crucial role in depression resistance, as it is positioned at the opposite end of the spectrum from depressive traits. To understand this relationship, we can break extraversion into its two primary facets: enthusiasm (gregariousness) and assertiveness.
Enthusiasm and Assertiveness as Protective Factors
Enthusiasm (Gregariousness):
High enthusiasm is protective against depression, as it is associated with stronger positive emotional responses and greater social support. Studies confirm that social engagement and positive affectivity act as buffers against depressive symptoms by fostering dopamine-related reinforcement mechanisms (Watson & Naragon-Gainey, 2014).Assertiveness:
High assertiveness contributes to greater goal-directed behavior and reduced passivity, decreasing vulnerability to depressive inertia. Assertiveness is linked to higher self-efficacy, which in turn lowers susceptibility to stress-induced depressive states (Judge & Bono, 2001).
SIVHs and Their Influence on Extraversion
Somewhat surprisingly, SIVHs can significantly influence an introverted person’s motivation to become more assertive and socially engaged. The key mechanism is reconceptualization — when an individual journals, reflects, and consciously works toward a higher aim, their perceived need for social interaction and dopamine-boosting activities (e.g., exercise, engagement) becomes more structured and meaningful.
Structured Goal-Setting Enhances Assertiveness:
Especially for conscientious individuals with low assertiveness, goal-setting within an SIVH framework can substantially increase assertiveness, as this sub-trait is relatively plastic. Research suggests that structured behavioral interventions can improve assertiveness over time, particularly when combined with self-monitoring and reward-based reinforcement (Anderson et al., 2014).Encouraging Proactive Behavior to Build Positive Momentum:
Breaking down the movement toward a higher aim into manageable steps fosters motivation and engagement, counteracting withdrawal-driven depression. Studies in behavioral activation therapy confirm that gradual exposure to proactive behaviors can systematically rebuild motivation and resilience against depressive states(Mazzucchelli et al., 2009).
SIVHs as Tools for Enhancing Enthusiasm and Assertiveness
Through SIVH implementation, we extensively work on both assertiveness and enthusiasm by:
✔ Encouraging journaling and structured goal-setting to reinforce motivation for social interaction.
✔ Using structured rewards and milestone-based progress tracking to boost assertiveness.
✔ Breaking down proactive behaviors into manageable steps to counteract depressive inertia.
✔ Integrating dopamine-releasing activities (e.g., exercise, meaningful social interaction) within the SIVH framework to create positive reinforcement loops.
Some of the References used for the Article
Anderson, T., McClintock, C. G., & Gale, M. M. (2014). Improving assertiveness through behavioral training: A meta-analytic review. Psychological Bulletin, 140(3), 532–556. Link
Baumeister, R. F., Vohs, K. D., & Tice, D. M. (2007). The Strength Model of Self-Control. Current Directions in Psychological Science, 16(6), 351-355. Link
Carver, C. S., Johnson, S. L., & Joormann, J. (2008). Serotonergic function, two-mode models of self-regulation, and vulnerability to depression: What depression has in common with impulsive aggression. Psychological Bulletin, 134(6), 912-943.
Castrén, E., & Hen, R. (2013). Neuroplasticity as an antidepressant target. Nature Reviews Neuroscience, 14(7),471-484.
Dantzer, R., O’Connor, J. C., Freund, G. G., Johnson, R. W., & Kelley, K. W. (2008). From inflammation to sickness and depression: when the immune system subjugates the brain. Nature Reviews Neuroscience, 9(1), 46-56.
Decety, J., & Cowell, J. M. (2014). The complex relation between morality and empathy. Trends in Cognitive Sciences, 18(7), 337-339. Link
Deci, E. L., & Ryan, R. M. (2000). Self-Determination Theory and the Facilitation of Intrinsic Motivation, Social Development, and Well-Being. American Psychologist, 55(1), 68-78. Link
DeYoung, C. G., Peterson, J. B., & Higgins, D. M. (2010). Sources of openness/intellect: Cognitive and neuropsychological correlates of the fifth factor of personality. Journal of Personality, 78(2), 825-858. Link
DeYoung, C. G., Quilty, L. C., & Peterson, J. B. (2007). Between facets and domains: 10 aspects of the Big Five. Journal of Personality and Social Psychology, 93(5), 880-896.
Godlewska, B. R., & Harmer, C. J. (2021). Serotonin and depression. Neuropsychopharmacology, 46(1), 220-230.
Greenberg, J., Pyszczynski, T., & Solomon, S. (1997). Terror Management Theory of Self-Esteem and Cultural Worldviews: Empirical Assessments and Conceptual Refinements. Advances in Experimental Social Psychology, 29, 61-139. Link
Gross, J. J. (2015). Emotion Regulation: Conceptual and Empirical Foundations. Annual Review of Psychology, 66, 1-26. Link
Higgins, E. T. (1987). Self-Discrepancy: A Theory Relating Self and Affect. Psychological Review, 94(3), 319-340. Link
Hofmann, S. G., Sawyer, A. T., Fang, A., & Asnaani, A. (2012). Emotion regulation in generalized anxiety disorder, social anxiety disorder, and their co-occurrence. Journal of Anxiety Disorders, 26(1), 134-141. Link
Hudson, N. W., & Fraley, R. C. (2015). Volitional personality trait change: Can people choose to change their personality traits? Journal of Personality and Social Psychology, 109(3), 490-507.
Jackson, J. J., Hill, P. L., Payne, B. R., Roberts, B. W., & Stine-Morrow, E. A. (2012). Can an old dog learn (and want to experience) new tricks? Cognitive training increases openness to experience in older adults. Psychology and Aging, 27(2), 286-292.
Kashdan, T. B., & McKnight, P. E. (2013). Commitment to a purpose in life: An antidote to the suffering by individuals with social anxiety disorder. Emotion, 13(6), 1150-1159.
Kotov, R., Gamez, W., Schmidt, F., & Watson, D. (2010). Linking ‘big’ personality traits to anxiety, depressive, and substance use disorders: A meta-analysis. Psychological Bulletin, 136(5), 768-821.
Krishnan, V., & Nestler, E. J. (2008). The molecular neurobiology of depression. Nature, 455(7215), 894-902.
MacLeod, A. K., & Moore, R. (2000). Positive thinking revisited: Positive cognitions, well-being and mental health. Clinical Psychology & Psychotherapy, 7(1), 1-10.
Miller, A. H., & Raison, C. L. (2016). The role of inflammation in depression: from evolutionary imperative to modern treatment target. Nature Reviews Immunology, 16(1), 22-34.
Nestler, E. J., Barrot, M., & Dileone, R. J. (2002). Neurobiology of depression. Neuron, 34(1), 13-25.
Pariante, C. M., & Lightman, S. L. (2008). The HPA axis in major depression: classical theories and new developments. Trends in Neurosciences, 31(9), 464-468.
Sapolsky, R. M. (2001). Depression, glucocorticoids, and hippocampal atrophy. Annals of the New York Academy of Sciences, 933(1), 67-77.
Santarelli, L., Saxe, M., Gross, C., Surget, A., Battaglia, F., Dulawa, S., & Hen, R. (2003). Requirement of hippocampal neurogenesis for the behavioral effects of antidepressants. Science, 301(5634), 805-809.
Widiger, T. A., & Oltmanns, J. R. (2017). Neuroticism is a fundamental domain of personality with enormous public health implications. World Psychiatry, 16(2), 144-145.
Willner, P., Scheel-Krüger, J., & Belzung, C. (2013). The neurobiology of depression and antidepressant action. Neuroscience & Biobehavioral Reviews, 37(10), 2331-2371.